APC UPS Replacement Battery Kits - ap 885-4514e
B-mode is the single most important mode you need to master in order to be proficient at point of care ultrasound (POCUS). All of the other modes rely on you getting a good B-mode (2D) image. Fortunately, we already discussed the most common ultrasound settings for B-mode in the ultrasound Knobology section above.
The rule of thumb is to only use as much depth that is necessary to see your structure of interest. Often times for beginning users, their depth will be too high and there is a lot of wasted “Ultrasound Real Estate” on the bottom of the screen.
2230683. Award Instrument: Cooperative Agreement. Program Manager: Mike Pozmantier mpozmant@nsf.gov (703)292-4475. ITE Innovation and Technology Ecosystems TIP ...
Thirty-eight studies reporting the GTR rates with the different surgical guidance techniques were included in the network meta-analysis. The network chart of the meta-analysis is shown in Figure 2. Direct comparisons suggested that the rate of GTR (rGTR) is better with iMRI than with neuronavigation, 5-ALA, and conventional surgery, and those of 5-ALA and neuronavigation were better than that of conventional surgery [Table 1]. The heterogeneity was moderate overall, though most comparisons showed high heterogeneity. A node-split analysis was used to evaluate the consistency between the direct and indirect comparisons [Table 2]. The results showed that there was a slight inconsistency in the comparisons between iMRI and neuronavigation/conventional surgery. The results of the consistency model for the network analysis are shown in Figure 3. The random model was selected because of the high heterogeneity. The posterior probabilities of the five methods of surgery were ranked as follows: MRI > iUS ≈ 5-ALA > neuronavigation > conventional surgery [Figure 4].
In the past decade, there has been great interest in the use of iMRI because it can provide highly valuable information and real-time feedback on the extent of resection and presence of residual neoplasm during image-guided tumor resection. High-field MRI with an integrated neuronavigation system has been found to provide reliable anatomic and functional data during surgery.[62] The real-time visualization of the space between the white matter fiber tracts and the tumor helps the surgeon avoid the tract, which should reduce the risk of neurological deficits, particularly in the case of infiltrating tumors such as gliomas.[62] Napolitano et al.[22] reported opposite results demonstrating that iMRI improved the quality of resection and the GTR. Our data supported the idea that the use of iMRI could help neurosurgeons achieve the goal of extensive but safe tumor resection. However, the limitations of iMRI are its high cost and the time it adds to a surgery. Moreover, it is an offline method, meaning that its use requires pausing the surgery to assess the results.[63] iMRI scan prolongs the time of surgery, which may lead to an increase in postoperative complications. The most relevant risks were correlated with pressure- and heat-related skin damage because of the prolonged surgery time and possible heating of the patients in the iMRI scanner.
First, we conducted a pair-wise meta-analysis of studies by comparing the same interventions with a random-effects model[9,10] to combine the conclusions of different studies. Forest plots were used to assess the statistical heterogeneity.[11] The analysis was conducted using Review Manager, version 5.3 (RevMan 5; The Cochrane Collaboration, 2015).
Rocking the ultrasound probe involves “rocking” the ultrasound probe either towards or away from the probe indicator along the long-axis.
It is the ideal probe for cardiac scanning however it can perform all of the applications the curvilinear probe can as well (with less lateral resolution).
The most common POCUS applications for the endocavitary ultrasound probe are for intraoral (peritonsillar abscess) and transvaginal applications (early pregnancy, ovarian torsion, ovarian cyst, fibroids, ectopic pregnancy, etc). Make sure to always place a sterile endocavitary probe cover (condom or glove) prior to scanning.
A total of 2842 related studies were obtained in the initial search, and 38 studies from 1980 to 2018 were included for the network meta-analysis[15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52] [Figure 1].
Here is a video demonstrating all of these Pulse Wave Doppler steps to calculate the Velocity Time Integral of the left ventricular outflow tract:
In general, for almost all standard applications and procedures the indicator orientation marker position will be on the LEFT side of the screen. In cardiac mode, the indicator orientation marker will be on the RIGHT side of the screen.
Nineteen studies reported information about postoperative complications with four different technologies. The network chart is shown in Figure 5. During the surgical resection of a brain tumor, various complications might occur such as aphasia, epilepsy, and dyskinesia. On direct comparisons, MRI was better than neuronavigation and conventional surgery, and neuronavigation was better than conventional surgery [Table 1]. The heterogeneity was moderate, and there was a slight inconsistency for the MRI and conventional surgery data according to the network meta-analysis [Table 2]. The results of the consistency model showing the different comparisons are shown in Figure 6. Thus, the following ranking was derived: conventional surgery > neuronavigation > iMRI > iUS [Figure 7].
1Department of Medical Imaging, Cancer Hospital of China Medical University, Liaoning Cancer Hospital and Institute, Shenyang, Liaoning Province, China
The impact of intraoperative technologies on the rate of postoperative complications is a valid end point in addition to GTR. Previously published study data did not provide a direct comparison among the four guidance technologies and conventional surgery for glioma resection. Because of the limited number of studies reporting postoperative complications, we included only iMRI, iUS, neuronavigation, and conventional surgery. The ranking results showed that conventional surgery had the worst performance in terms of the incidence of complications, whereas iUS was the best followed by iMRI and neuronavigation. Our data implied that iUS and iMRI may decrease the rate of complications following glioma surgery. However, there was a slight inconsistency in the network meta-analysis: in the direct comparison of iMRI and conventional surgery, the OR and 95% CI were 0.36 and (0.19, 0.65), respectively, whereas those in the pooled comparison were 0.24 and (0.14, 0.42), respectively. Based on the direct comparison, it was clear that iMRI was superior to conventional surgery, and the pooled comparison exaggerated the difference between them. Thus, the ranking results were confirmed. Based on this finding, iUS appears to be the safest tool used in the resection of gliomas as it reduces the risk of postoperative complications. iUS has the advantage of real-time scanning and offers the ability to differentiate blood in the resection cavity or marginal resection from residual tumor. In addition, iUS can help surgeons observe lesions in multiple directions and can be repeated many times during the surgery to enable accurate tumor resection, which is considered to lead to reduced postoperative complications. There were three included studies comparing iUS to other guidance technologies. Thus, the network analysis was based on direct and indirect comparisons. However, more studies are needed to verify the conclusion based on a large sample size.
The most common Doppler mode you will use is color Doppler. This mode allows you to see the movement of blood in arteries and veins with blue and red patterns on the ultrasound screen.
Calipers are an important feature of ultrasound machines that allows you to measure the distance of specific structures of interest.
5-ALA is based on the fluorescence of protoporphyrin IX accumulating in glioma cells, acting as a biological tag of these cells; this makes it easy for the surgeon to locate, observe, and resect the glioma while avoiding damage to other brain tissues.[57] One of the important and undisputed values of protoporphyrin IX spectroscopy is that it can facilitate the standardization of ALA-fluorescence image-guided neurosurgery (FIGS) compared with the human eye, which has wide variations in color perception; it might be particularly useful for color-blind surgeons.[74] A single-arm meta-analysis of eight studies reported that the specificity of 5-ALA-fluorescence image guided surgical resection was 88.8%, and its sensitivity was 82.6%.[57] Thus, more and more clinical trials have been done to seek the US Food and Drug Administration approval for the use of 5-ALA in malignant glioma resection.[75] 5-ALA-based imaging is limited by heterogeneity within the tumor and signal attenuation in necrotic and malignant areas, making it difficult for surgeons to recognize the lesions. Yet, ALA-FIGS offers a great advantage in that it is easy to learn and integrate into practice.[76] Because there are no two-arm studies comparing ALA-FIGS with other technologies, unfortunately, ALA was not involved in the outcomes of postoperative complications and clinical improvement, so a comprehensive assessment could not be made.
When you are in one of these Doppler settings, you will be able to optimize your image further by adjusting the following ultrasound buttons/knobs:
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
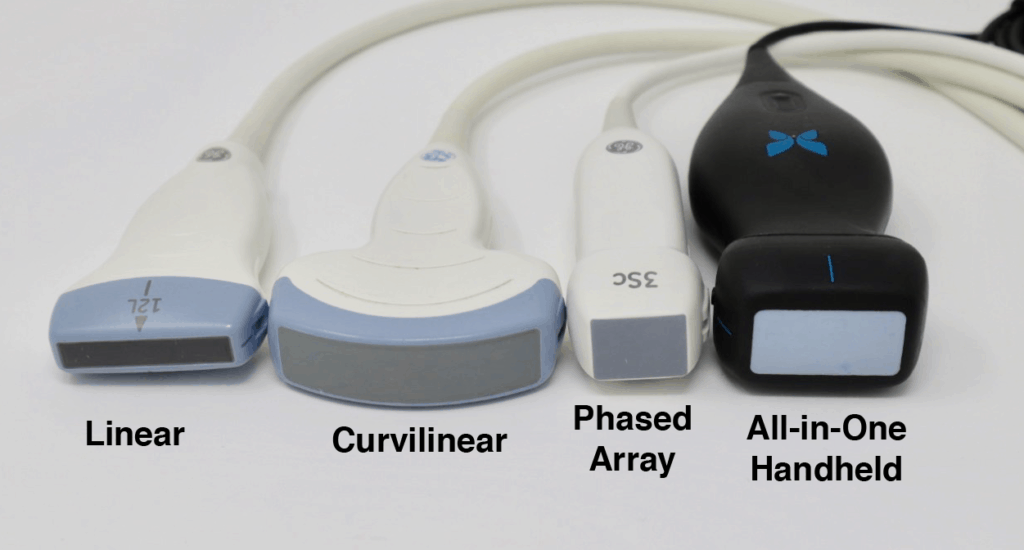
The images below demonstrate the relative sizes and footprints of the 3 most commonly used ultrasound probes (Linear, Curvilinear, and Phased Array):
The results of our network meta-analysis suggest that image-guided surgery may be more effective than conventional surgery for tumor resection and support the use of iMRI, iUS, 5-ALA, and neuronavigation as valuable tools for glioma surgery. However, large randomized clinical trials are required to further elucidate the true value of image-guided surgery.
Most other ultrasound machines will allow you to further adjust the gain in even more specific areas of your ultrasound screen. This ultrasound setting is called “Time Gain Compensation” or TGC.
Modern technologies are highly advanced to guide surgeons during glioma resection. Our network meta-analysis elucidated the added value of different technologies for surgical guidance in patients with gliomas in terms of rGTR, postoperative complications, and clinical improvement.
The advantage of this probe is that piezoelectric crystals are layered and packed in the center of the probe making it easier to get in-between small spaces such as the ribs (notice the extremely small pinpoint footprint on the ultrasound image below).
[…] Para obtener cada punto de referencia en las vistas discutidas a continuación, la sonda de ultrasonido a menudo necesitan ser manipulados en un número de orientaciones. […]
After switching to the correct ultrasound probe, the next step is to select the correct application preset for that transducer.
I would suggest approaching any ultrasound machine in with the following order using the step-by-step approach below. I’ve found doing it in this order prevents you from forgetting to optimize basic ultrasound settings that can drastically improve your image quality.
Gliomas are the most common brain tumors in the world.[1] Surgery is one of the most effective therapeutic methods in terms of patient prognosis. It has been reported that the gross total resection (GTR) and extent of resection are closely correlated with the 5- and 10-survival rates.[2] However, according to the characteristic infiltrative nature of malignant gliomas, it can be challenging to fully resect these tumors.[1] In the past three decades, several visual guidance technologies have been used to achieve maximum resection while maintaining patient safety. These technologies include intraoperative magnetic resonance imaging (iMRI), intraoperative ultrasound (iUS), fluorescence-guided surgery with 5-aminolevulinic acid (5-ALA), and intraoperative neuronavigation.[3,4,5] There is no doubt that a prospective double-blinded randomized controlled trial would be the next ideal step to compare these technologies with conventional surgery. However, the execution of such trials is impractical because of logistical, financial, and ethical reasons. To date, there has been no uniform standard in terms of the overall benefits for patient survival and postoperative complications in the central nervous system and other systems to compare these technologies. In clinical practice, it remains difficult for neurosurgeons and health-care providers to select the appropriate imaging technology to gain the most support. Therefore, in this study, we compared different guidance techniques with conventional surgery for glioma resection in terms of GTR, postoperative complication rate, and postoperative clinical improvement, which are often considered the most important factors in the surgical resection of gliomas. We used multiple treatment meta-analyses[6] combining the evidence of direct and indirect comparisons.[7] The objective was to provide an informative conclusion that can help improve clinical practice.
The name of the first author, study design, year of publication, number of patients in each group, and major outcomes were collected from each article. The Newcastle–Ottawa Quality Assessment Scale[8] was used to evaluate the quality of each included article.
[…] Further reading: 1. Enriquez JL and Wu TS. An introduction to ultrasound equipment and knobology. Crit Care Clin. 2014 Jan;30(1):25-45, v. doi: 10.1016/j.ccc.2013.08.006. 2. Wiafe YA and Badu-Peprah. The Influence of Ultrasound Equipment Knobology in Abdominal Sonography. In: Essentials of Abdominal Ultrasound, Gamie SAA and Foda EM (ed.) [online] 2019. DOI: 10.5772/intechopen.83713 3. Dinh V. Ultrasound Machine Basics-Knobology, Probes, and Modes. Pocus 101 [online] https://www.pocus101.com/ultrasound-machine-basics-knobology-probes-and-modes/#B-Mode_Brightness_Mod… […]
The combination of image guidance modalities in glioma resection is a popular trend. These multimodal approaches theoretically facilitate complete tumor resection as well as the preservation of neurological function.[78] We hope that high-quality studies using multivariate analysis will be conducted in future to evaluate the combination of multiple technologies in glioma surgery.
TITUS S.S. Lunch Box with Lid - 500 ml. Add to List. Delivery & Returns. AED 39 Save AED 0 Earn 15 Shukrans What is Shukran? Shukran is the Landmark Group's ...
Tilting the ultrasound probe involves moving the transducer from side to side along the short axis of the probe. It is commonly also called “Fanning” as well. Tilting will allow visualization of multiple cross-sectional images of a structure of interest. You can apply this technique to structures such as the heart, kidney, bladder, vessels, etc.
However, if a machine does allow you to adjust the focus, it is very important to place the focus cursor to the depth of the area of interest. Usually, the focus is indicated by a small arrow (or hourglass) superimposed on the depth markings.
This is why you can’t use this mode for very high-velocity applications such as severe regurgitation or stenosis of the heart valves. Here is an example of aliasing with pulse wave Doppler:
Sliding involves moving the entire probe in a specific direction to find a better imaging window. This is usually used to find the best window, move to different areas of the body, or to follow a specific structure (such as a vessel).
Gliomas are the most common type of brain tumor in the world. Surgical resection is one of the most effective therapeutic methods in terms of patient prognosis. However, it is difficult for neurosurgeons and health-care providers to select which imaging technology to best support the procedure. These technologies included intraoperative magnetic resonance imaging (iMRI), intraoperative ultrasound (iUS), fluorescence guidance with 5-aminolevulinic acid (5-ALA), and intraoperative neuronavigation. Hence, in this study, we compared the gross total resection (GTR), postoperative complications within or outside of the central nervous system, and postoperative clinical improvement by multiple meta-analyses, which allows the integration of data through direct and indirect comparisons.
The most important outcome measures were the rates of GTR, postoperative complications, and clinical improvement. The GTR was defined as the percentage of cases resulting in ≥90% tumor removal as measured via postoperative magnetic resonance imaging (MRI) within a week after surgery. The postoperative complication rate was defined as the percentage of patients that experienced complications of the central nervous system, such as neurological deficits, epilepsy, cognitive deficits, and aphasia, and those outside the central nervous system, such as infection, thrombosis, and cerebrospinal fluid leakage. The clinical improvement rate was defined as the percentage of patients that were in stable condition during the follow-up examination. A dichotomous outcome was utilized in this network meta-analysis: we used the number of patients whose brain tumors were totally resected, who experienced postoperative complications, and who experienced significant clinical improvement or were stable at least 3 months after surgery.
iMRI, iUS, neuronavigation, and conventional surgery were compared in terms of patients' clinical improvement. Our data confirm that iMRI was superior with respect to this metric, followed by iUS and neuronavigation; all were better than conventional surgery. There was consistency between the direct and indirect evidence in the node-split analysis. These data suggested that iMRI was the best technology for the clinical improvement of patients. The risk factors for negative results were prior surgery or radiotherapy.[61]
If you read the beginning of this post, you should already know what ultrasound probe you need to use based on the application you are performing. So after turning on the ultrasound machine, the next most important step is to switch to the correct ultrasound transducer you will need.
Initially, these Doppler modes may seem confusing but in reality, all Doppler settings are simply meant to detect speed going either Towards or Away from your probe (check out our previous post on Doppler Physics HERE). Understanding this is the first step to mastering ultrasound Doppler.
Address for correspondence: Prof. Haozhe Piao, Department of Neurosurgery, Cancer Hospital of China Medical University, Liaoning Cancer Hospital and Institute, Shenyang 110042, Liaoning Province, China. E-mail: [email protected]
Here is what the Curvilinear probe looks like and how an ultrasound image will appear on the screen. Notice the curved nature of the ultrasound image.
B-Mode (Brightness Mode) in ultrasound is a setting that creates a two-dimensional (2D) greyscale image on your ultrasound screen and is the most commonly used mode. It is also commonly called 2D mode.
However, there are now handheld devices that connect to your smartphone and can simulate multiple probe types with just a click of the button. The Butterfly Ultrasound Device is an example of this (see below). From my experience, the footprint is slightly larger than the phased array and the weight of the probe is about 2-3 times more than a typical phased array. This increased weight is accounted for by the processor and the battery.
Below is an example of how the M-mode (left side of screen) and B-mode (right side of screen) compare when looking at lung sliding. M-mode simply takes a “slice” of your B-mode image where the cursor line is placed and translates that “slice” over time. It ignores everything else on the B-mode scan except for where you have that cursor line. You can see on the Y-axis how the structures (subcutaneous tissue, muscle, and pleural line) correlate between the M-mode and B-mode images. You can also see the relative motion of these structures over time (X-axis).
The PubMed, Cochrane Library, Web of Science, Embase, China Knowledge Resource Integrated Database, and WanFang databases were searched for publications before April 2018. Randomized controlled trials, two-arm and three-arm prospective studies, and retrospective studies in patients who underwent surgical treatment for glioma were included. The most important outcome measures were the rates of GTR, postoperative complications, and clinical improvement.
Ultrasound gain simply means how bright or dark you want your image to appear. It increases or decreases the strength of the returning ultrasound signals that you visualize on the screen.
The commonly used Sonosite M-Turbo or Edge machines allow you to adjust the “Near field” and “Far field” gain of your ultrasound images. The near field refers to the top half of the ultrasound screen and the far field refers to the bottom half of the ultrasound screen. The overall gain is just called “Gain” and is on the bottom left-hand corner of the Sonosite machine buttons.
If you went through the previous steps then you should have a really good and optimized image. Here are just some other buttons you may encounter that may be useful if you need to freeze, measure, or capture your ultrasound image.
Each transducer will have a different list of application presets based on its frequency and footprint. The ultrasound device companies will create application presets that make sense for those specific probes.
I would suggest that if you are just starting out, focus on B-mode (greyscale), and get really good at obtaining high-quality 2D images. After you feel comfortable with B-mode start adding on and learning the other more advanced Doppler modes. You can always come back to this post as a reference when you are ready to use the other modes!
The steps to performing continuous wave Doppler are the similar to Pulse wave Doppler except where you put the sample gate does not matter. It will measure velocities across the entire cursor line.
POCUS 101 Tip: Sometimes, you may be in a different mode or ultrasound machine setting and may wonder how to just reset your settings. Usually pushing the B-mode or 2D button on the ultrasound machine will reset everything and bring you back to the simple B-mode setting.
Compression with the ultrasound probe involves putting downward pressure on the probe to evaluate the compressibility of a structure or organ of interest. The most common use is to evaluate for deep vein thrombosis, differentiate between artery versus vein, and evaluation for appendicitis (non-compressible).
Eleven studies reporting clinical improvement and return to stable condition with four technologies were included [Figure 5]. From the direct comparisons, iMRI was better than neuronavigation and conventional surgery [Table 1]. The absence of obvious heterogeneity and inconsistency suggests that these data can be used in the network meta-analysis. The comparisons based on the consistency model. The ranking was determined as follows: iMRI > iUS > neuronavigation > conventional surgery [Figure 8].
Neuronavigation has been used in routine glioma surgery.[77] It helps to visualize the tumor borders and results in shorter surgical times and smaller craniotomies.[77] It is usually based on preoperative CT or MRI images, so the main limitation of neuronavigation is that the preoperative images are not as accurate once brain tissue is removed during the surgery. Some studies have shown the positive impact of neuronavigation in glioma surgery, whereas most reports provided questionable evidence.[77] Our meta-analysis supported the latter view and found that neuronavigation performed worse than other technologies.
All ultrasound machines will allow you to save an image and/or video clip of your ultrasound scan. This is important if you are trying to archive, bill, or use any ultrasound images/videos as teaching files.
The last ultrasound setting you can use to optimize your image is by adjusting the focus. When you adjust your focus you are simply concentrating your ultrasound waves at a specific depth of the image to maximize the resolution at that depth.
Ultrasound M-mode is defined as a motion versus time display of the B-mode ultrasound image along a chosen line. The motion is represented by the Y-axis and time is represented by the X-axis. Common applications for M-mode include looking at E point septal separation in cardiac scanning or calculating fetal heart rate for obstetrics. You can also use M-mode in lung ultrasound to evaluate for lung sliding and rule out pneumothorax.
I hope you found this post helpful! Here is a Video summarizing the most commonly used ultrasound knobs, probes, and modes:
The phased array (or sector array) transducer is commonly branded as the “cardiac probe” and has a frequency range from 1-5MHz. It has a similar frequency range as the curvilinear probe but has a smaller and flat footprint.
Handling the ultrasound probe and proper movement is essential to obtaining optimal ultrasound images. There are traditionally 4 basic movements that are performed when scanning with ultrasound they are Slide, Rock, Tilt(Fan), Rotate. Another technique that could be considered a “5th” cardinal movement is Compression.
In this post we will go over the 4 most common Point of Care Ultrasound probes you will encounter (linear, curvilinear, phased array, and endocavitary probes). The table below lists when you should think about using each type of ultrasound probe.
Now the application preset will usually give you a decent image right when you place the ultrasound probe on the patient. However, there are some ultrasound settings that may need to be adjusted to optimize your ultrasound settings further.
It is very important that you master each of these ultrasound transducer manipulation/movement techniques. Most experienced sonographers think what manipulation or combination of movements will give them the desired image. In their minds, they know how each transducer manipulation should change their image. With deliberate practice, you will be able to do this too!
There is a mode similar to color Doppler that you may encounter called Power Doppler. This mode does not show up as red or blue on the screen but only uses a single yellow color signifying the amplitude of flow. So you can’t tell if the flow is going towards or away from the probe given that it has only one color. It is more sensitive than color Doppler and is used to detect low flow states such as venous flow in the thyroid or testicles.
The “probe indicator” on the ultrasound probe can be identified as an orientation marker (ridge, indentation, groove, or nub) on one side of the probe. This corresponds to the indicator or orientation marker on the ultrasound image.
Rotating the ultrasound probe involves turning the transducer in a clockwise or counterclockwise direction along its central axis. Rotation is most commonly used to switch between the long and short axis of a specific structure such as a vessel, the heart, the kidney, etc.
Accessing the Tissue Doppler function will vary by machine but usually just involves pushing a knob/button labeled “TDI” (Tissue Doppler Imaging) while you are in the Pulse Wave Doppler mode.
(Editor’s note: I’m using the velocity of blood as the example here. But the same principles apply if you are measuring muscle movement using tissue doppler.
One of the most important assumptions behind the network meta-analysis is coherence, which means that the direct and indirect evidence do not disagree beyond chance.[13] A node-split analysis was used to assess the consistency of the direct and indirect evidence for each loop in the network.[14] The node-split and network analyses were both run in R version 3.5.0.
POCUS 101 Tip: For learners, really trying to improve, I always suggest that when you see a suboptimal image, think to yourself what is the next best transducer manipulation you can perform to get an optimal image. Too often, learners try a random combination of transducer movements without thinking first what the image should look like prior to manipulating the transducer.
Selecting the correct application preset is similar in that it will automatically select the ideal frequency, depth, and gain for that application (i.e. cardiac vs abdominal). This gives you a great starting point to further fine-tune your image with the other knobs/buttons (depth, gain, focus, TGC, etc). In addition, the ultrasound will always start in B-mode or “greyscale” mode by default.
It should be noted that our meta-analysis is limited by the quality of the underlying studies upon which it was based. However, a significant benefit of network meta-analyses is that large amounts of information can be aggregated, leading to higher statistical power and stronger point estimates than is possible from the measures derived from any individual study. Other limitations of our meta-analysis include the small sample size of some studies, relatively short follow-up, and the inconsistent use of various adjuvant therapies. Subgroup analyses were not performed, but future studies could investigate the effects of different tumor stages, different tumor histologies, adjuvant chemotherapy, patient age, MRI field strength, or tumor location. Another limitation was that six studies defined GTR as resection of 95% or 98% rather than 100%; these variations in the definition were permitted because there is no clinically significant difference between 100% and 98% tumor resection.[54] Although scientists, economists, and health-care policymakers would like to see prospective random studies comparing these technologies, such a study would be practically challenging because these technologies are complementary to each other and are generally used in combination. However, this analysis is of great clinical value as it provides insight into the benefit of image guidance with respect to the GTR, postoperative complications, and clinical improvement. Yet, our study and the limitations of the published literature emphasize the need for larger studies to evaluate the importance of imaging-guided technologies for treating gliomas.
The endocavitary probe has a curvilinear footprint with a wide view but has a much higher frequency (8-13 MHz) than a curvilinear ultrasound probe. The image resolution of the endocavitary probe is exceptional, but like the linear probe, it must be adjacent to the structure of interest since it has such a high frequency/resolution, but poor penetration.
Think of selecting the ultrasound application preset like how you would select the correct preset for your point and shoot camera. You would use a different setting for day mode versus light mode. The camera will help adjust the settings to optimize for those specific conditions.
So the most important thing you can do to improve your technique for any Doppler mode is to make sure that the movement/speed of whatever you are measuring is parallel to your ultrasound probe as much as possible (zero degrees). Anything above 25-30 degrees will significantly underestimate your measurements. And if you are perpendicular, the cosine of 90 degrees = 0 and the ultrasound Doppler will read no flow or movement.
The first of these ultrasound settings you should adjust is the depth. The ultrasound depth setting is simply how deep you want the ultrasound machine to be able to scan.
Radiographically, the body is divided into three distinct planes: Sagittal, Coronal, and Transverse. Any combination of those movements is considered “Oblique.”
Considering the rGTR, it has been demonstrated that the complete resection of a tumor is related to better survival.[53,54,55,56] Hence, it is wise for surgeons to use intraoperative guidance technologies to achieve maximal safe surgical resection. We also compared these guidance technologies with conventional surgery (i.e., surgery without any image guidance technology) as a control to evaluate the benefit associated with each technology. The GTR was defined based on the postoperative MRI within 1 week after surgery as described previously.[57,58] The results showed that iMRI was associated with the best GTR, followed by iUS, 5-ALA, and neuronavigation; the GTR was the worst with conventional surgery. There was a slight inconsistency with iMRI and neuronavigation and conventional surgery in our network meta-analysis. We tried to evaluate whether the slight inconsistency could influence the posterior probability ranking of the five methods. We found that the OR and 95% confidence interval (CI) in direct comparison of iMRI and neuronavigation were 3.21 and (2.34, 4.38), respectively, while those in the pooled comparison were 3.00 and (2.10, 4.50), respectively. Moreover, the 95% CIs mostly overlapped. These findings support the fact that iMRI was better than neuronavigation in terms of the GTR and does not affect the ranking derived from the network meta-analysis. In the pooled comparison, we just shortened the gap between iMRI and neuronavigation, however, the inconsistency did not affect the rank of neuronavigation. The position that neuronavigation was ranked second to last followed by conventional surgery could be verified both in direct and pooled comparisons. In the direct comparison of iMRI and conventional surgery, the OR and 95% CI were 3.11 and (1.53, 6.30), respectively, while those in the pooled comparison were 5.70 and (3.40, 9.60), respectively. In the direct comparison, it was clear that iMRI was better than conventional surgery, but the pooled comparison exaggerated the gap between them. The Cochrane Handbook suggests that direct comparisons can be regarded as accurate when both direct and indirect evidence exist.[59] It has been suggested that the outcomes of direct and indirect comparisons are not always the same.[60] If the direct comparison is not convincing, an indirect comparison can provide a useful supplement. As it is not possible to perform direct comparisons among all of these intraoperative guidance technologies in the clinic, this network meta-analysis offers the advantage of combining direct and indirect comparisons to rank the different methods.
Here is an example of measuring tricuspid regurgitation (TR) using continuous wave Doppler. Notice how CW Doppler can measure the high velocity of this TR jet (344cm/s).
Rocking allows you to help center the area of interest. This is also referred to as “in-plane” motion because the image is kept in-plane throughout the manipulation.
This power symbol applies to almost all ultrasound devices as well. Just look for it when you want to turn on your machine.
(Editor’s note: for the Butterfly. You don’t actually have to switch between transducers because it is an “all-in-one” device. When you switch the application preset it will automatically simulate the correct transducer settings for you)
The good news is that all of the principles of Pulse Wave Doppler also apply to Tissue Doppler. In fact, Tissue Doppler is just another form of Pulse Wave Doppler that allows you to measure the much slower speeds of tissue/muscle movement (from 1cm/s – 20cm/s) compared to Pulse Wave Doppler that measures the much faster speed of blood (30cm/s – 200cm/s).
Just like the world implies, the “freeze” button freezes a frame for you so you have time to view it in more detail. The ultrasound machine will usually store a 10-30 seconds of data and you can scroll back to see previous frames as well.
Below is a quick video demonstrating how to use all of these functions (freeze, measure, image capture) by measuring the LVOT (left ventricular outflow tract) diameter. You can use this same technique to measure any other structure of interest.
by K Zöller · 2024 · Cited by 1 — Polymers that fulfill all these criteria and succeeded in clinical trials and/or as commercial product are therefore excellent examples for the design of new ...
2Department of Neurosurgery, Cancer Hospital of China Medical University, Liaoning Cancer Hospital and Institute, Shenyang, Liaoning Province, China
These views can be obtained by rotating 90 degrees relative to each other. These terms are helpful in structures such as vascular and cardiac applications. Also, this is useful when deciding to perform a procedure in a short versus long-axis approach.
Facts to compare and choose whether to buy running shoes New Balance Fresh Foam 1080 v7 vs HOKA Mach 6, by viewing the online comparison side by side.
Conversely, if you decrease the depth you will be visualizing more superficial structures. Here is an example below of decreasing depth:
Product Title: Corsair 32GB (2x16GB) Dual Channel Vengeance RGB Black (DDR5 6000/30/1.40v) - CMH32GX5M2B6000C30 KSN SKU Code: MB125396
This is really great ,it has cleared my basic concepts and lessen the confusion of handling the machine which nobody teaches this way. Kindly guide how can I connect with you for further guidance regarding ECHO. Kind Regards.
All ultrasound machines will have an “Overall” Gain setting that, when increased or decreased, will make the entire ultrasound image brighter or darker. This is good to use when your entire imaged is too dark (under-gained) or too bright (over-gained).
Here is an example of the long axis and short axis of the heart. The parasternal short axis is obtained by rotating 90 degrees clockwise from the parasternal long axis view.
Each ultrasound probe will have it’s pros and cons. Usually, the most important factors to decide on are resolution, penetration, and footprint size. Here is a figure showing how penetration and resolution are affected with respect to the frequency of the transducer.
In this post, I will go over the most common Ultrasound Knobology (knobs/buttons), Probes, Modes, Movements, Orientations, and Planes you will need to properly scan. By learning these ultrasound basics, you will be able to have the fundamentals on how to use any ultrasound machine you may encounter!
The developed ranking probability table indicated that iMRI was superior in terms of the GTR and clinical improvement, while iUS was the least likely to result in postoperative complications. Hence, it was concluded that iMRI or iUS is the most advantageous imaging modality.
Tel: 0208 741 7471 Out of Hours and Emergencies 111 is the NHS non-emergency number. It's fast, easy and free. Call 111 and speak to a highly trained ...
(Editor’s note: Regarding this section, we are referring to Gain in the setting of B-mode/greyscale. You can also change the gain in your Doppler modes which we will discuss in the following section on “Advanced Modes.” Lastly, some machines have an “Autogain” button that I rarely use because I find it typically undergains your image.)
Pulse Wave (PW) Doppler allows you to measure the velocity of blood flow (at a single point). A unique aspect of Pulse Wave Doppler is that you can specify to the ultrasound machine exactly where you would like the machine to measure the velocity using the Sample Gate. It’s usually seen by two horizontal lines along your cursor. you can move your cursor and your sample gate and place it exactly where you want to measure your blood velocity.
The medical literature in PubMed, Cochrane Library, Web of Science, Embase, the China Knowledge Resource Integrated Database, and the WanFang database was searched by using the medical subject heading (MeSH) terms “glioma,” “intraoperative,” “MRI,” “magnetic resonance imaging,” “ultrasound,” “ALA,” “5-aminolevulinic acid,” “neuronavigation,” “conventional surgery,” “image guidance,” and “neurosurgery” in different combinations. All of the databases were searched up to April 2018. Randomized controlled trials, two-arm and three-arm prospective studies, and retrospective and prospective studies in patients with glioma who received surgical treatment were included. Single-arm studies and studies that did not completely report the outcomes of interest were excluded. Reviews, letters, comments, editorials, case reports, and personal communications were excluded. Two independent reviewers screened each article, and if there was uncertainty regarding eligibility, a third reviewer was consulted. The references in each included article were double-checked to ensure that all related articles were included.
Unlike Pulse Wave Doppler which has a sampling gate to measure a single point along your cursor, Continuous Wave Doppler measures all points along your cursor. Therefore what you will see will be the maximum velocity of flow detected along the cursor line. This is a pro and a con. It is a pro because you don’t have aliasing and can detect high velocities, but it is a con because you don’t know exactly where that velocity is coming from on the cursor. Also if there are two velocities along the cursor line, you won’t be able to differentiate the lower velocity compared to the higher velocity signal, since the high-velocity signal will mask the low-velocity one.
All Doppler signals (regardless of which Doppler mode you are using) are calculated using the Doppler Shift Equation. Below is a figure detailing how the Doppler Shift is used and how the angle of insonation is extremely important in what the transducer will detect as the speed of flow/movement. For any type of Doppler, you want the flow/movement to be going directly towards your probe (zero degrees). As you move more towards a 90-degree angle there will be no flow detected by the ultrasound machine.
The Ultrasound Probe “Footprint” refers to the area on the probe that comes in contact with the patient’s skin in order to produce an ultrasound image. It is located at the very tip of the probe and is usually has a soft “rubbery” feel. Depending on the application you may want a smaller or larger footprint. Regarding footprint width from largest to smallest it goes: Curvilinear > Linear > Phased Array.
A common question that comes up with color Doppler is: What do the colors on ultrasound mean? The answer is: RED means there is flow TOWARDS the ultrasound probe and BLUE means that there is flow AWAY from the ultrasound probe. It is a misconception that red is arterial and blue is venous. It actually just depends on the direction blood is flowing relative to the angle of your ultrasound beam.
The single most important factor that will determine if you can get proper ultrasound images is choosing the correct ultrasound probe or transducer. Like with anything else you do, the right tool will be needed for the right situations. For example, if you used a linear probe, that has great resolution but minimal depth, you will not be able to visualize much if any of the heart.
Now it may seem daunting when thinking about all of the available ultrasound modes available. In this section, the most common and basic ultrasound modes: B-mode and M-mode. In the following section, I will cover the more advanced Doppler Modes.
This is an interesting fact: the on and off buttons were derived from a binary numbering system where “0” was for OFF and “1” was for ON. So to create the universal symbol for Power the “0” and “1” were combined to make the following symbol:
The use of cranial US was previously limited by the probe size because it was too big for access via the opening made by a craniotomy, and the images were not very clear compared with computed tomography (CT) or MRI.[58] In the recent few decades, however, these issues have been addressed: the imaging quality has improved greatly with three-dimensional acquisition and advanced computer technology, and the probe size has become more suitable for craniotomies.[58] The most significant development in iUS was the introduction of a probe for superficial lesions (7.5–10 MHz) and deep lesions (3–5 MHz).[64] To the best of our knowledge, the most notable remaining problem is that brain shifting during surgery, which can vary from 2 to 25 mm depending on the lesion location and size,[65] cannot be avoided. The results of the meta-analysis of the single-arm studies indicated that the postoperative neurological status was worse in patients with iUS: 11.3% (range from 8% to 13%) of patients exhibited no postoperative neurological improvement and 19% were better off.[58,60,66] Furthermore, studies have shown that there were no more durable deficits when iUS was used alone than with conventional surgery.[47,67] Both iMRI and iUS can correct for errors caused by brain shift, but the limitation with US arises from the reduction in quality and resolution of the imaging because of artifacts associated with the resection procedure.[68] The sensitivity, specificity, and positive and negative predictive values of US were the greatest at the start of surgery (95%, 95%, 98%, and 90%, respectively), as surgery proceeded the four values decreased to 88%, 42%, 73%, and 67%, respectively, and 26%, 88%, 62%, and 62%, respectively, at the end of the surgery.[58] Another issue with iUS is that surgeons must be familiar with the anatomic orientation, though some strategies have been developed to mitigate this.[69] It is important to note that the benefits of MRI and US are highly dependent on the skill and experience of the surgeon. Another limitation of US is that it cannot be used in some cases depending on the size or location of the skull opening.[57] However, when we perform craniotomies, iUS is used for planning the surgical incision and identifying the important surrounding structures.[70] Direct comparisons between iUS and iMRI are not always possible. However, a few studies have been done to compare the sensitivities and specificities of these technologies. One study comparing two-dimensional iUS with low-field MRI among 26 patients showed that MRI outperformed iUS.[71] Another study comparing high-field MRI with linear-array US in 44 Grade II astrocytoma biopsy specimens showed that the specificity was 67% for both technologies, and the sensitivity of MRI was higher than that of US (83% versus 79%).[72] In another study, the sensitivity of US and MRI was 75% and 55%, respectively, and the specificity was 58% and 96%, respectively.[73] Our study reported that MRI was clearly the best tool for surgical guidance, but considering the high cost of MRI, iUS is an acceptable alternative.
Properly performing Point of Care Ultrasound involves understanding the ultrasound knobs, machine, and equipment. But you may have issues finding a resource that allows you to easily learn how to understand and use the ultrasound machine.
In the example below, we are going from a short axis to the long axis of the brachial artery by rotating clockwise 90 degrees:
Now some learners may feel like the “other doppler modes” such as Pulse wave, Continuous wave, and Tissue Doppler are very advanced settings. However, the same principles of color Doppler apply to these other Doppler modes as well. The ultrasound probe is just detecting flow or motion either TOWARDS or AWAY from it. If flow/motion is towards the probe there will be a positive deflection and if it is away from the probe there will be a negative deflection.
Conventional surgery without imaging assistance is not widely used for the sake of patient outcomes. Most of the data related to conventional surgery and other technologies included in this network meta-analysis were obtained from the China Knowledge Resource Integrated Database and the WanFang database. The data showed that the outcomes of conventional surgery were notably different from those of imaging-guided surgery. The outcomes of conventional surgery are greatly dependent on the surgeon's experience in recognizing the brain tissue, blood vessels, and nerves. This finding was supported by our meta-analysis: conventional surgery was ranked the lowest in terms of all the three metrics evaluated. Hence, we recommend the use of image guidance technology if the cost is acceptable.
The biggest limitation with Pulse Wave Doppler, however, is that there is a limit on the maximum speed you can detect. Anything past this limit (termed Nyquist Limit) will cause the signal to alias. In general, you do not want to use Pulse Wave Doppler for any applications that require measuring speed above 200cm/second.
24 Mar 2021 — Question: This question is designed to be answered without a calculator. sec x tan x dx = 4x 7 - sec X+C 8x2 O -tan x + c 8x2 7 16x4 ...
Continuous Wave Doppler is very similar to pulse wave Doppler except it does not alias and can detect very high velocities (greater than 1000cm/second). So Continuous Wave Doppler is the optimal choice for measuring high-velocity applications such as valvular stenosis and regurgitation.
Adjusting the Time Gain Compensation (TGC) allows you to adjust the gain at almost any depth of your ultrasound image, not just the near and far-fields. The top rows of the Time Gain Compensation control the nearfield gain and the bottom rows control the far-field gain.
Besides B-mode and M-mode you will have other advanced ultrasound Modes that involve “Doppler.” Here is an image of all the available ultrasound modes:
Then, we generated a random-effects model within a Bayesian framework using Markov chain Monte Carlo methods in R version 3.5.0 (R Foundation for Statistical Computing, Vienna, Austria).[7,12] The model incorporated the outcomes of the different interventions used in each study to assess the relations between these technologies in terms of odds ratios (ORs).[6] This model combined the direct and indirect evidence for all compared interventions. Thus, the technologies were ranked based on the OR for each outcome measure compared with over several iterations of the Markov chain. We could get the ranked probability of four technologies and conventional surgery in different outcome measures by calculating the OR for each surgical method compared with an arbitrary common control group, counting the proportion of iterations of Markov chain in which each method had the highest OR, the second highest, and so on.
Below we are rotating between a short-axis and long-axis of the brachial artery using a clockwise rotation of 90 degrees.
(Editors Note: There is some more recent literature that suggests that the term “sliding” should indicate motion along the long axis of the probe and “sweeping” involves motion along the short axis of the probe. However, I have found this confuses learners more than just the general term sliding to encompass any movement of the probe from the original position. Also sometimes when you are sliding you are not just going along the short or long axis of the probe but a combination. However, I wanted to mention this distinction in case you encounter it)
Duracell Ultra Lithium Pack of 2 · Capacity: 1500 mAh · Battery Chemistry: Lithium · Warranty: 1 YEAR.
Περιγραφή Σταθμού: Ο 88μισό πανω απ΄όλα είναι ένα μουσικό ραδιόφωνο που προσεγγίζει τις σύγχρονες τάσεις με ένα πολυσυλλεκτικό τρόπο.
Most ultrasound machines will have settings that allow you to fine-tune and adjust the gain at specific depths of your greyscale ultrasound image. These will be termed Near/Far field gain or Time Gain Compensation (TGC).
This post mainly goes over ultrasound machine settings, probes, buttons, and functions. I also created another post on a simple way of learning Ultrasound Physics and Artifacts you can access by clicking HERE.
[…] knobs/buttons (depth, gain, focus, TGC, etc). In addition, the ultrasound will always start in B-mode or “greyscale” mode by […]
Backup Medical can supply replacement parts for your medical equipment. These replacements include batteries, hand controls, actuators/motors and trolley ...
The linear ultrasound probe is a high-frequency transducer (5-15 MHz) that will give you the best resolution out of all of the probes but is only able to see superficial structures. A general rule of thumb is that if you are going to ultrasound anything less than about 8cm, then use the linear probe. Anything above 8cm you won’t be able to see much.
[…] get the Aortic Valve level from the Mitral Valve level, tilt the tail of the probe inferiorly and point it towards the Aortic […]
5-Aminolevulinic acid; conventional surgery; glioma; intraoperative; magnetic resonance imaging; network analysis; neuronavigation; resection; ultrasound
Here is an example of decreasing the TGC of the middle of the image with a corresponding absence of echoes on the middle of the ultrasound screen.
The curvilinear ultrasound probe has a frequency range of 2-5MHz. It is considered a low-frequency probe and has a large/wide footprint, allowing for better lateral resolution (compared to the phased array probe). The curvilinear ultrasound probe is often used for abdominal and pelvic ultrasound exams. However, it can also be used for cardiac and thoracic ultrasound exams but is limited by the large footprint and difficulty with scanning between rib spaces.
This seems like common sense but I’ve seen many learners just want to jump in and start scanning with the wrong transducer. Unfortunately, understanding all of the ultrasound knobs won’t mean much if you have the wrong ultrasound probe to start off with!
The good news is that all ultrasound machines have the same basic settings and once you understand them you can start using any ultrasound device with ease.
The right side of the screen will have dots or lines that correspond to the depth in centimeters. This can give you an estimation of how deep your structures are as well. As you INCREASE the depth setting on your machine, you will see the numbers increase on the right side of the screen to correspond to the depth of penetration.
In terms of GTR, iMRI (odds ratio [OR] = 5.70, 95% confidence interval [CI]: 3.40–9.60), iUS (OR = 2.70, 95% CI: 1.10–6.90), 5-ALA (OR = 2.40, 95% CI: 0.64–8.90), and neuronavigation (OR = 1.90, 95% CI: 1.20–3.10) were found to be more effective than conventional surgery. In addition, iUS (OR = 0.15, 95% CI: 0.04–0.52), iMRI (OR = 0.24, 95% CI: 0.14–0.43), and neuronavigation (OR = 0.34, 95% CI: 0.18–0.56) were more found to result in fewer complications than conventional surgery. Furthermore, patients' clinical improvement was better with iMRI (OR = 8.10, 95% CI: 3.00–25.00), iUS (OR = 4.90, 95% CI: 0.76–33.00), and neuronavigation (OR = 2.60, 95% CI: 1.00–7.20) than with conventional surgery.



 Neil
Neil 
 Neil
Neil