'I'm 89 and owe £4800 in tax – but HMRC won't let me pay' - 4800 60
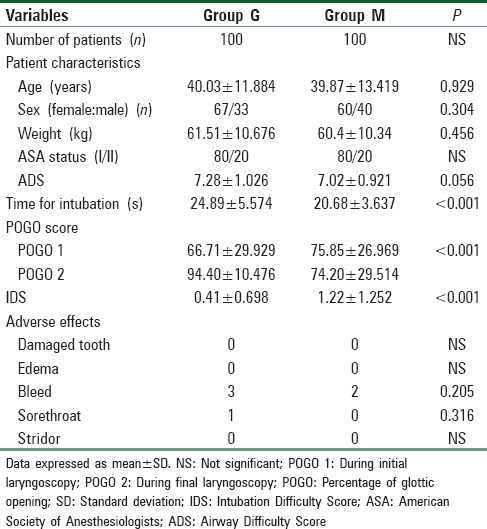
Based on the previous studies, a projected difference of 10% between the groups for first attempt success rate, a type I error of 0.05 and a power of 0.9, a total of 200 patients were studied. To accommodate for dropouts 220 patients were enrolled. The data were analyzed using Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA version 15.0 for Windows). Post hoc power analysis was done using Univariate Analysis of Variance test. For parametric data paired t-test and Mann–Whitney U-test was used and for nonparametric data Chi-square test was used. The intragroup comparison between CL grades during initial and second laryngoscopy was done using McNemar-Bowker test and for POGO scores Wilcoxon Signed-rank test was used. The ADS and IDS were compared in each group with Pearson's product-moment correlation. Results were considered statistically significant for P < 0.05.
Securing and maintaining the airway and respiration in a safe and apt manner is of prime importance in anesthesia practice. This caters to both routine and difficult intubations, whether anticipated or unanticipated. A recent review of adult and pediatric perioperative cardiac arrests reports airway management as the cause of anesthesia-related cardiac arrests in over half of the cases.[1] The majority of tracheal intubations performed routinely are easy and effortless, depending on the experience of the anesthesiologist, techniques, equipment, and airway manipulations. Difficult airway may be prevented by adequate preoperative evaluation, accomplished by various measurements of anatomical landmarks or noninvasive clinical tests. However, the success of such evaluation is limited and difficult tracheal intubation still occurs in 1.5%–8.5% of general anesthetics and may result in complications, the most serious being hypoxemic brain damage and death.[2] Conventionally, endotracheal intubation (ETI) is performed using a Macintosh laryngoscope which involves distortion, compression, and manipulation of anatomical structures to achieve adequate glottis view. Still, the intubation difficulty occurs in 1%–4% and failure results in 0.05%–0.35% cases.[3] The present study aimed to evaluate and compare GlideScope with Macintosh laryngoscope for ease of ETI in adult patients undergoing elective surgery under general anesthesia. GlideScope is a video laryngoscope (GVL), which utilize the video technology and fiberoptic system to provide a continuous display of the image on external monitor and these do not require line of sight view of larynx also GVL has a blade with 60° angulation providing a wider field of view.[4,5]
The ADS was compared with the IDS in both groups using Pearson's product-moment correlation. The R value was calculated as 0.205 in Group G (correlation significant at 0.05 level) and 0.601 in Group M (correlation significant at 0.01 level).
Mounting, engine KAVO PARTS EEM-4585. Fitting Position: Right. Weight: 0.000 kg. Price From (Excl. VAT). €85.74. Add to cart ...
The primary step during any laryngoscopy manoeuvre is the visualization of the glottic opening, which thus implies the use of higher forces for adequate visualization of glottic opening especially in a difficult airway scenario. These excess forces have a direct effect on the hemodynamic response to ETI. The blade of GlideScope is inserted orally in the midline and does not require alignment of the oral, pharyngeal, and laryngeal axis. It follows the anatomical upper airway without the need of displacement of tongue to align the optical axis and thus a lesser degree of lifting forces and tissue distortion for the optimal laryngeal view. With significant reduction in these forces, as proved by a multitude of studies, one expects lesser forces, and lesser chances of injury with GlideScope especially while intubating a potential difficult airway.[22] Russel et al. in 2012 compared lifting forces required during GlideScope and Macintosh laryngoscope in 24 patients and found significantly lower peak (9N vs. 20N), average (5N vs. 11N), and impulse (9N vs. 150N) lifting force required with GlideScope when compared with Macintosh laryngoscope, respectively.[23] This study revealed a significant increase in pressor response in Macintosh group when compared with the GlideScope group [Figures 1 and 2]. The findings of the present study is in agreement with a similar study published in 2010 comparing hemodynamic changes with ETI in 200 adult male patients undergoing elective orthopedic surgery under general anesthesia.[24] Our results are in contrast to study by Pournajafian et al. found there was no significant difference between pressor response to intubation through GlideScope or direct laryngoscopy as they found that TTI was significantly long with GlideScope and stimulation due to the passage of tracheal tube through the vocal cords has a greater impact on blood pressure and heart rate than that due to the laryngoscope.[25] The results of the present study suggest intubation through GlideScope reduces the mechanical stimulus to oropharyngolaryngeal structures during ETI especially useful for high-risk cardiac or neurosurgical patients.
Thus, the results of present study show that GlideScope offers superiority over Macintosh laryngoscope by providing better laryngeal views (CL grade and POGO) and improved intubation difficulty scores with lesser hemodynamic response during routine intubation in an unselected population.
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
CL grading was described for conventional laryngoscopy using Macintosh blade; hence, the magnified and indirect view of glottis through GlideScope does not fit into the criteria of CL grading. Hence, POGO score was proposed it is better as it is a continuous numeric scale.[21] The glottic exposure in itself is not a true reflection of ease or difficulty during ETI, especially with the use of GlideScope as numerous studies report improvement in laryngoscopy grade but difficulty in passage of endotracheal tube. This requires a more objective and qualitative assessment and scoring of difficulty in intubation with use of IDS which suggested intubation to be easier in group G as compared to group M. The ADS was compared with the IDS in both groups using Pearson product-moment correlation. The R value was calculated as 0.205 in group G (correlation significant at 0.05 level), and 0.601 in group M (correlation significant at 0.01 level) showing preoperative determination of ADS could successfully predict difficulty encountered during ETI.
... 1<- <1EJT5(RYM@>:&M6T^,*+HQ7IGQ3(<+'RH[?+$,>(.R(O'0P;$ M<'L%8EE>! 9&;,[(H30<>[O1.G,11WG"I/$UP_MF.DK-K,\5R8&VLC@&!Q() MXFDM')H7<<>*D&D02VPG?6@&G&0 ...
A new scoring system has been developed during recent years, airway difficulty score comprising of thyromental distance, mallampati grading, mouth opening, neck mobility, and upper incisors. A score between 5 and 15 is given for each patient and a score ϭ8 is considered potentially difficult intubation
Studies have shown an improvement in POGO scores using GlideScope by Choi et al. (67.6 ± 24.7–89.6 ± 20.0) while intubating normal airways and Kim et al. in simulated difficult airway scenario.[17,19] A systemic review and meta-analysis by Griesdale et al. projected an improved glottis visualization using GVL as compared to direct laryngoscopy especially in anticipated or simulated difficult laryngoscopy. Furthermore, there was an improved, successful first intubation attempt and faster TTI with GVL, but it was confined to studies of nonairway expert operators.[20]
Groups with close to 200k members can be converted to a Broadcast Group that allows unlimited members. Only admins can post in Broadcast Groups, but everyone ...
Hemodynamic parameters revealed a higher pressor response to ETI in Group M as compared to Group G. In Group G, three patients and in Group M, two patients had minor lip and tongue bleed and only one patient in group G had sore throat, which was found to be statistically and clinically insignificant [Table 1].
The mean POGO scores during initial and final laryngoscopy were 66.71 ± 29.929 and 94.40 ± 10.476 in Group G and 75.85 ± 26.969 and 74.20 ± 29.514 Group M. The difference in mean POGO scores during final laryngoscopy between two groups was statistically highly significant (P < 0.001). Intragroup analysis revealed significant improvement in POGO scores between initial and final laryngoscopy with 70 patients showing improvement of scores in Group G (P < 0.001). In Group M, only 15 patients showed improvement of scores whereas 28 patients had worsening of scores [Table 1].
Address for correspondence: Dr. Anudeep Jafra, Department of Anaesthesia and Intensive Care, Postgraduate Institute of Medical Education and Research, Nehru Building, 4th Floor, B Block, Chandigarh - 160 012, India. E-mail: anu_gmch@yahoo.co.in
Nellcor Covidien DS100A SpO2 Original ; SMITH BCI, 3100, 3180, 3300, , 3302, 3303, 3401, 6100, 9100 ; WELCH ALLYN, 1500, 42NT0-E1 LXi, ATLAS 6200 , ENCORE 202EL, ...
The difference in time for intubation was found to be more in Group G (P < 0.001) which was statistically significant but clinically not relevant as there was no effect on patients’ oxygenation status. Studies show conflicting reports due to nonuniformity of definition for TTI and level of expertise. Our study is in agreement to Sun et al. and Xue et al. which also found that time to intubate through GlideScope was longer than direct laryngoscopy.[8,9] The increased TTI in group G was probably due to use of standard four-step insertion technique and use of rigid nonmalleable stylet in GlideScope which requires manipulation.[5]
A new scoring system proposed by Adnet et al., called intubation difficulty scale (ids) which is a quantitative scale of intubation difficulty and claimed to be useful for objectively comparing the complexity of endotracheal intubations. The IDS is a blend of subjective and objective criteria that permits a qualitative and quantitative approach to the progressive nature of the difficulty of intubation. It can easily be calculated by the operator or an independent observer. It requires recording of seven parameters:
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Item # 6505. Gloves Bamboo Fit Purple Medium. $10.99. Item # 6505. In Stock. We currently have 2 in stock. Add to Cart. 1, 2. Bamboo Fit gloves are the perfect ...
The rate of successful endotracheal intubation (ETI) in both groups was 100% in the first attempt. The time required for successful ETI was 24.89 ± 5.574 in Group G and 20.68 ± 3.637 in Group M (P < 0.001) found to be statistically significant. There was significant improvement in glottic view with GlideScope (as assessed by POGO score 66.71 ± 29.929 and 94.40 ± 10.476 in group G and 75.85 ± 26.969 and 74.20 ± 29.514 Group M and CL grading [P < 0.001]). A comparison of mean IDS between two groups revealed intubation was easier with the use of GlideScope. The hemodynamic response to intubation was significantly lesser with the use of GlideScope when compared with Macintosh laryngoscope. The incidence of adverse events, though minor like superficial lip or tongue bleed, was similar in two groups.
Center Disk, Fits Brand Dayton, For Use With Grain... Replacement Parts, Parts, RFQ · 4TK04, 4TK04, Machine Vise, Drill Press Vise, Fixed Base, 6 in J...
The prospective, randomized, controlled study was conducted to compare the ease of intubation, Cormack–Lehane grading (CL), percentage of glottis opening (POGO), and pharyngolaryngeal morbidity between the Macintosh and GlideScope videolaryngoscope in adult patients undergoing elective surgery under general anesthesia.
Rate of successful intubation in either group was similar (100% in first attempt). No patient had failed insertion or use of alternative techniques for intubation and ventilation. This is in agreement with previous studies by Sun et al. (95.5%), Xue et al. (97%) and Aziz et al. (97%).[8,9,10] In the present study, first laryngoscopy was done by trained anesthesiologist and second by person trained in both techniques and experience of more than 30 intubations with GlideScope that accounted for higher first-time success rate. In contrast to our study, Choi et al. found that there was no significant difference in first-attempt intubation success and failure rates between GVL and Macintosh groups in patients intubated in emergency department. Problems encountered in GVL were due to its steep blade curvature. Furthermore, the glottic view was impaired by condensation of water vapor on the lens or due to mucus, blood, or vomit which resulted in failure to intubate.[11] Another study by Ibinson et al. found a greater first-attempt success rate for intubation when using the GlideScope versus direct laryngoscopy. Authors also found that GlideScope was 99% successful for intubation after initial failure through direct laryngoscopy, helping to reduce the incidence of failed intubation.[12]
Numerous studies have previously reported an improvement in CL grading. Some of these studies have been done in predicted or simulated difficult airways[13,14,15,16] while others in general patient population and normal airways[8,9,16,17,18] and findings of the present study further confirms and extends this evidence.
Many studies show variable incidence of sore throat after laryngoscopy with either GlideScope or Macintosh laryngoscope. A few published case reports about tonsillar, soft palate, pharyngeal injury due to GVL have also come through.[26] This is attributed to the rigid nonmalleable style (The GlideRite® Rigid Stylet), and apparent blind spot (just below the tip of the blade) as the endotracheal tube is advanced into mouth and when it finally appears on the screen. Lesser incidence of such complications in our study might be attributed to the use of predefined standard and safe anesthetic technique, ensuring adequate depth of anesthesia and using standardized techniques of insertion. Similar incidence of minor trauma has been reported by Xue et al. and Aziz et al.[9,10]
Time to intubation (TTI) was measured from the insertion of device into the mouth to obtaining a square wave capnogram on monitor. In case of failure to intubate change of blade, use of external manipulation, and alternative devices use was allowed and number of attempts to intubation was recorded and these patients were excluded from analysis. Ease of intubation was assessed through TTI, number of attempts and glottis view and intubation difficulty score [IDS-Annexure 2] 17 was also recorded.[7] All vital parameters were recorded every 1 min during intubation and every 5 min till 15 min after intubation. The following complications were recorded broken teeth, bleeding gums, and presence of sore throat, stridor, and hoarseness of voice in postanesthesia care unit.
The modified CL grade during initial laryngoscopy and final laryngoscopy was I/IIa/IIb/III in 26/51/18/5 and 73/27/0/0 patients in Group G and was I/IIa/IIb/III in 45/41/13/1 and 45/42/09/04 in Group M. The difference during final laryngoscopy between the two groups was statistically highly significant (P < 0.001). Intragroup analysis in Group G revealed significant improvement in CL grade in 37 patients between first and final laryngoscopy (P < 0.001), whereas in Group M only 3 patients showed improvement which was not significant [Tables 2–4].
The aim of the study was to compare the ease the intubation using GlideScope video laryngoscope and Macintosh laryngoscope in adult patients undergoing elective surgery under general anesthesia.
Our results suggested that GVL offers a better laryngeal view and improved IDS when compared with Macintosh laryngoscope for routine ETI.
Hemodynamic parameters blood pressure (statistically significant – diastolic blood pressure at NIBP3, NIBP4, NIBP5 and systolic blood pressure at NIBP4). Nibp: Noninvasive blood pressure
There are certain limitations in our study. First, to minimize the bias due to lack of blinding two operators was used on the same patient who was blinded to either's laryngoscopy scores. Further, this study was performed in the American Society of Anesthesiologists I/II patients posted for elective surgery; the intubating conditions might be different in emergency, awake, obstetric, and critical care setting. The present study was not adequately powered to predict the impact of GVL in an actual difficult airway situation which requires a larger sample size. Furthermore, all insertions were performed by an experienced user and our results may not be extrapolated to users with limited experience with the device.
Glottis view was assessed using modified CL grading and POGO scoring during initial laryngoscopy and intubation. The results of present studied showed a significant improvement in laryngoscopy views in GVL group when compared between two groups and in intragroup comparison between scores of initial and final laryngoscopy hence strengthening the role of video laryngoscopes in difficult airway scenarios.
After obtaining the institutional ethics committee approval of Government Medical College and Hospital (in accordance with Helsinki declaration), (Trial registered in Clinical Registry Trials-India, CTRI/2013/08/003889), and written and informed consent 200 patients of either sex, age group of 18–60 years, American Society of Anesthesiologists physical status I and II, undergoing elective surgery requiring general anesthesia with ETI were enrolled. Patients who were morbidly obese (body mass index >35 kg/m2), with known airway pathology, with increased risk of aspiration, pregnancy, coagulopathy or history of anticoagulant use, cardiovascular or cerebrovascular disease, and cervical spine injury were excluded from the study. Patients were randomly allocated to one of the two groups (GVL [Group G] and Macintosh laryngoscope [Group M]) using computer-generated random number tables and coded sealed envelope method. All patients underwent preoperative airway examination and airway difficulty score [ADS-Annexure 1] a day before surgery.[6] In the operating room, standard monitoring included pulse oximetry, noninvasive arterial blood pressure, electrocardiography, and capnography (S/5™ Datex Ohmeda USA). General anesthesia was induced after three minutes of preoxygenation using propofol 2–2.5 mg/kg in 50% oxygen and nitrous and isoflurane (concentration 0.5%–1%). After ensuring adequate bag-mask ventilation rocuronium 0.6 mg/kg was given for muscle relaxation and analgesia was achieved using 2 μg/kg of fentanyl. Injection Lidocaine 1.5 mg/kg was given 90 s before intubation to decrease pressor response to laryngoscopy. Initial direct laryngoscopy (Macintosh blade 3) was done in all patients by an independent laryngoscopist and laryngoscopic findings (CL grade and POGO score) were noted. Second laryngoscopy was done by other laryngoscopist who was blinded to previous observations and laryngoscopy was done as per group allocation either using GVL blade 3 or 4 and Macintosh blade 3 and laryngoscopic findings were noted. No external laryngeal manipulation was used and the difference in laryngoscopic findings was recorded.
GlideScope offers superiority over Macintosh laryngoscope in terms of laryngeal views and the difficulty encountered at ETI in an unselected population.
Suzuki Clutch Bell Ver1 (Sand Blast) is Now on Stock! JVT Philippines 0922 844 0336 0917 836 8680 0949 8872900 # 129 8th ave. St. cor. D. Aquino St....
As healthcare's leading source of the knowledge, processes and components ... partssource-inc: N/A. AfterShip logo. AfterShip for Shoppers. Get real-time ...
The mean IDS was 0.41±0.698 and 1.22 ± 1.252 in group G and M respectively which was found to be statistically significant thus indicating intubation was easier in group G (P < 0.001) [Table 1].
A total of 200 American Society of Anesthesiologists I–II patients of either sex, in the age group of 18–60 years were included in the study. Patients were randomly allocated to two groups. We assessed ease of intubation depending on time to tracheal intubation, number of attempts, glottic view (Cormack–Lehane grade [CL grade] and percentage of glottis opening [POGO]) and intubation difficulty score (IDS), hemodynamic variables and any intra- and post-operative adverse events.
773656. Part #:. Alternate Item ID: Part No desc: Description: Pump Set Epump Bag Set NO Flush Kangaroo Epump Bag Set 1000cc NO Flush Bag. Kangaroo Epump Bag ...
Opens the Configure representation dialog in which you specify the part and part reference properties to be displayed in the table in the left-hand section.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Patient demographic characteristics were found to be similar in two groups. First attempt success rate of intubation was similar in Group G and M (100%, 100%). The mean intubation time was 24.89 ± 5.574 in Group G and 20.68 ± 3.637 in Group M which was statistically significant (P < 0.001) [Table 1].



 Neil
Neil 
 Neil
Neil